What is cystic lung disease?
Cystic lung disease is a term used to describe four distinct conditions that may share a degree of common origin during fetal development. These conditions are:
Bronchogenic cysts (also called a bronchopulmonary foregut malformation)
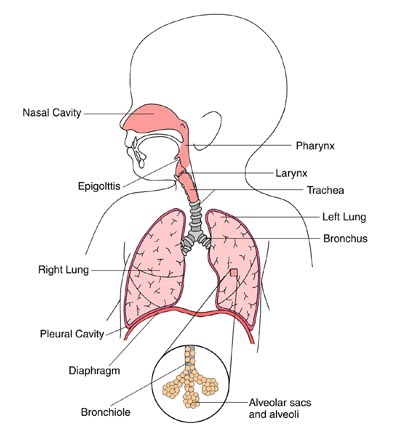
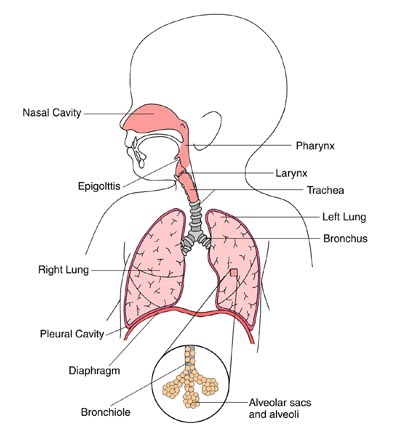
- This is a cyst usually found on midline chest structures of the body, such as the esophagus and trachea.
- They are sometimes also found on the lower lobes (sections) of the lung.
- Some of these cysts may become infected or grow so large that they compromise the function of the adjacent airway.
Cystic adenomatoid malformation (CCAM)
- This is a benign (non-cancerous) mass of abnormal lung tissue, located usually on one lobe of the lung.
- This condition is caused by overgrowth of abnormal lung tissue that may form fluid filled cysts or result in the failure of the development of the tiny air sacs that characterize a normal lung. The tissue does not function as normal lung tissue.
- There are two types of CCAMs: Type I is distinguished by one or more large cysts, and type II has both solid regions and cysts.
Lobar emphysema
- This is a condition that involves an obstruction in a lobe of lung that causes airflow to become trapped during inflation and expiration of the lungs.
- It may be congenital (present at birth) or acquired (not present at birth).
- It may affect only a part, but more often the entire lobe is involved, usually the left upper lobe.
- The obstruction of air flow causes the lung to distend (stretch out and expand). Depending on the extent of distension, the affected lobe can compress the unaffected lobe below or above it, and/or the opposite lung by extending across the mediastinum (the area that separates the lungs and houses vital structures such as the heart and major vessels).
- Without treatment, this condition can cause acute respiratory distress and even circulatory collapse.
Pulmonary sequestration
- This is a mass of nonfunctioning pulmonary (pertaining to the lungs and respiratory system) tissue.
- This kind of mass is subdivided into two types: extralobar or intralobar.
- An extralobar sequestration is typically located just above or just below the diaphragm. It is separated from the lung and enveloped by its own pleura (membrane that covers the outside of the lung).
- An intralobar sequestration is typically found in the lower lung lobes, more often on the left side, and is characterized by recurrent respiratory infections.
- Sequestrations can interfere with normal circulation, cause respiratory infections and/or lead to heart failure.
The Center for Healthy Infant Lung Development (CHILD) at Boston Children's Hospital cares for newborns, infants and children with many different forms of lung disease. Program expertise ranges from care of premature infants to care of full-term infants with breathing difficulties.
We offer a comprehensive, team-based approach to maximize the growth and development of the lungs, which helps children reach their maximum potential in all aspects of their normal activities, including exercise, feeding and learning. Our staff is available 24 hours per day, 7 days per week, and we pride ourselves in how available we are to our families.
Symptoms & Causes
What are the symptoms of cystic lung disease?
While each child may experience symptoms differently, and while symptoms may depend on the condition causing the disease, some common symptoms include:
- breathing difficulty
- pain with breathing
- wheezing
- shortness of breath
- recurrent pneumonia
Symptoms of cystic lung diseases may resemble other conditions or medical problems. Always consult your child’s physician for a diagnosis.
Can cystic lung disease be detected prenatally?
Yes, sometimes. Ultrasound may reveal some cysts or conditions; other times, symptoms may not appear until your child is significantly older.
What treatments are available for cystic lung disease?
Bronchogenic cysts
Since a cyst may compress your child's airway, it is important that it be removed in a careful and controlled manner. Depending on your child's age, symptoms, and the location of the cyst, it may be possible to remove it via thoracoscopic (minimally invasive) surgery.
To help your child during surgery, the surgeon may include careful ventilation or even use extracorporeal membrane oxygenation (ECMO). This is a machine that takes over for the lungs, providing oxygen and respiratory support.
Even if your child isn't experiencing symptoms from the bronchogenic cyst, it should be removed to prevent long-term complications, including infection, bleeding or malignant degeneration.
CCAMs
There are several ways to treat symptomatic CCAMs. These include:
- surgical aspiration (fluid suctioning) of a cystic lesion
- removal of a solid mass or affected lobe during fetal
For lesions that seem to be regressing and are not producing further symptoms, your child's doctors will perform simple post-natal follow up, which will include careful chest imaging and potential delayed pulmonary resection.
Though this course of action is open to debate, some people choose to have these asymptomatic CCAMs removed because of the rare but reported cases of malignant degeneration in these lesions as the babies grow into adults.
A CCAM may also produce neonatal respiratory distress complicated by pulmonary hypertension, and such babies may require urgent neonatal operation and/or aggressive management of their acute respiratory failure including the use of extracorporeal membrane oxygenation (ECMO), a machine that takes over for the lungs, providing oxygen and respiratory support.
Lobar emphysema and pulmonary sequestration
For these conditions, surgery is almost always required to remove the affected lobe (called a lobectomy) in order to prevent further damage to the entire lung. If done promptly, surgical treatment is almost always successful, leaving little or no permanent impairment of breathing capability.
What is the long-term outlook for a child with a cystic lung disease?
Fortunately, children typically do well after the treatment of their cystic lung disease. If they have severe associated anomalies or if the normal lung development has been compromised, then the outcomes may be more limited.
If your child's physician suspects a cystic lung disease, the following tests may be performed:
- prenatal ultrasound
- chest computerized tomography scan of the lungs (CT or CAT scan): this is a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images of your child’s lungs.
- Chest x-ray. This is a diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones and organs of the chest onto film.
The four conditions of cystic lung disease may become symptomatic, or be discovered, at different times:
Bronchogenic cysts
The condition is usually discovered on a fetal ultrasound or a chest x-ray after your fetus or newborn demonstrates signs and symptoms of airway obstruction.
CCAM
- A CCAM may be a coincidental finding at fetal ultrasound or it may be diagnosed when an ultrasound is done on a fetus in distress.
- Whether cystic or solid, a CCAM can be life threatening to the fetus, leading to a mediastinal shift, impaired function of the heart and fetal hydrops (congenital heart failure). Therefore, if your child’s doctors detect a lesion prenatally, they will want to monitor it closely.
Lobar emphysema
- This condition is usually also discovered on a chest x-ray after your child demonstrates extreme difficulty and pain with breathing.
- These symptoms usually become apparent right after birth, but may be delayed for as long as five to six months in some patients. Other patients remain undiagnosed until school age or beyond.
- If the obstruction is not found on an x-ray, a bronchoscope may be used. For this procedure, the bronchoscope, a lighted tube, is passed down your child’s windpipe so that doctors can examine the bronchial tubes.
Pulmonary sequestration
- Extralobar sequestration is most often found coincidentally when your baby is a newborn because of the discovery of another anomaly, such as a diaphragmatic hernia.
- In contrast, intralobar sequestration is typically discovered when your child is somewhat older, and has a lobar pneumonia that does not clear up or that leaves a radiographic abnormality even after the infection has been successfully treated.